【摘要】 目的 观察白内障超声乳化吸除联合小梁切除术治疗青光眼合并白内障的临床疗效。
方法 回顾分析患青光眼白内障在我院行超声乳化白内障吸除人工晶体植入联合小梁切除术的患者82例(82眼)和行白内障囊外摘除人工晶体植入联合小梁切除术的患者52例(54眼),记录手术前、后的视力和眼压,记录手术并发症和滤过泡情况。术后随访至少3个月。
结果 两组术后1周和3个月矫正视力较术前明显提高,眼压较术前明显降低(P均<0.05)。两组间术后视力和眼压比较,差异无显著性(P>0.05)。术后3个月随访,眼压≥21mmHg者,超乳三联术组2眼,囊外三联术组4眼,两组比较差异无显著性(P>0.05)。手术并发症超乳三联术组明显低于囊外三联术组,差异有非常显著性(P<0.01)。两组术后均无严重并发症发生。
结论 超声乳化白内障吸除人工晶体植入联合小梁切除术,可安全有效治疗青光眼合并白内障,且效果优于白内障囊外摘除人工晶体植入联合小梁切除术。
【关键词】 超声乳化白内障吸除术;白内障囊外摘除术;小梁切除术;青光眼;晶体
【Abstract】 Objective To evaluate the clinical effect of trabeculectomy combined with phacoemulsification for treatment of glaucoma with cataract.Methods This retrospective study included 134 cataract patients (136 eyes) with glaucoma. Among them, 82 patients (82 eyes) underwent the combined surgery of trabeculectomy and phacoemulsification with posterior chamber intraocular lens (IOL) implantation (phaco group), 52 patients (54 eyes) underwent trabeculectomy combined with extracapsular cataract extraction (ECCE) and IOL implantation (ECCE group). Best-corrected visual acuity (BCVA) and intraocular pressure (IOP) of pre- and post-operation, postoperative bleb formation and postoperative complications were analyzed. All cases were followed up for over 3 months.Results In two groups, in 1 week and 3 months postoperation, the BCVA was obviously better and the mean IOP was distinctly lower than that of preoperation (P<0.05). There was no significant difference between the two groups in both BCVA and IOP postoperatively (P>0.05). In 3 months postoperatively, only two eyes’ IOP was ≥21mmHg in phaco group, and in ECCE group there were only four. The operative complications in phaco group were significantly less than that in ECCE group (P<0.05). No severe postoperative complications were revealed in all of operated eyes.Conclusion Trabeculectomy combined with phacoemulsification and posterior chamber intraocular lens implantation is a successful, safe and effective way of treatment for patients with glaucoma and cataract. It has an advantage over trabeculectomy combined with extracapsular cataract extraction and intraocular lens implantation.
【Key words】 phacoemulsification;extracapsular extraction;trabeculectomy;glaucoma; lenses
对同时患有青光眼和白内障的患者,近一、二十年来,多主张采取联合手术治疗,因为其一次手术解除两种病痛,既迅速恢复视力,又有效降低眼压[1]。 20世纪80年代文献开始报道白内障囊外摘除和人工晶体植入联合小梁切除术[2](以下简称囊外三联术),随着超声乳化手术的进展,联合手术也逐渐向小切口发展,20世纪90年代文献报道白内障超声乳化吸除和人工晶体植入联合小梁切除术[3](以下简称超乳三联术)。我院自90年代末期对青光眼合并白内障患者行超乳三联术,取得满意效果,现将其与我们此前开展的囊外三联术分析比较,报告如下。
1 资料与方法
1.1 一般资料 行超乳三联术组82例(82眼),男31例,女51例;年龄最大84岁,最小45岁,平均(68.30±10.51)岁。术前视力为光感~0.4,其中<0.1者49眼,0.1~0.4者33眼。术前眼压为13.35~71.03mmHg(1mmHg=0.133kPa),平均(35.66±13.52)mmHg。晶状体核硬度均≤Ⅳ级(Emery及Little分级标准)。诊断为白内障合并原发性闭角型青光眼30眼,原发性开角型青光眼36眼,继发性闭角型青光眼16眼。见表1。
表1 两组术前情况比较
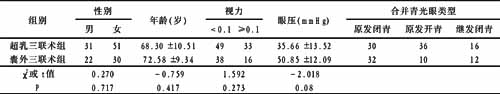
行囊外三联术组52例(54眼),男22例,女30例;年龄最大87岁,最小42岁,平均(72.58±9.34)岁。术前视力为光感~0.1,其中<0.1者38眼,0.1者16眼。术前眼压为32.97~81.78mmHg,平均(50.85±12.09)mmHg。诊断为白内障合并原发性闭角型青光眼32眼,原发性开角型青光眼10眼,继发性闭角型青光眼12眼。两组术前情况比较,差异无显著性(P>0.05)。
1.2 手术方法
1.2.1 行超乳三联术组 于上方作5mm×4mm巩膜隧道切口,切口两侧后端切开2mm,便于进入超声乳化针头和做小梁组织切除;根据晶状体核硬度分别使用拦截劈核法或原位超声法乳化吸出晶状体核,清除晶状体皮质,囊袋内植入一片式后房型人工晶体;作约1mm×2mm的小梁组织切除和虹膜根部切除,缝合巩膜瓣两角端各1针。
1.2.2 行囊外三联术组 于上方作5mm×4mm 1/2板层巩膜瓣,其两侧角膜缘各切开2.5~3mm,开罐式截囊,娩出晶状体核,清除晶状体皮质,植入一片式后房型人工晶体;作约1mm×2mm的小梁组织切除和虹膜根部切除,缝合切口。
1.3 术后治疗 两组常规术毕球结膜下注射地塞米松2.5mg,术后全身给予糖皮质激素和抗生素,第2天开放术眼,滴用糖皮质激素和抗生素眼液,必要时辅以球结膜下注射地塞米松2.5mg,3~5天出院。记录视力、眼压、眼底及手术并发症等。出院后继续滴用糖皮质激素和抗生素眼液1个月,逐周减少滴眼次数。定期随访。
1.4 统计学方法 本文数据采用SPSS 9.0统计软件包对计量资料和计数资料分别进行t检验、方差分析和χ2检验。
[1] [2] 下一页 |
